Published: March 17, 2024 | 11 mins read
Urine pH Role in Kidney Stone Formation
Our urine is composed of water, salts, and waste substances filtered out by the kidneys. The balance of these components can influence the alkalinity or acidity of urine, which doctors assess using pH. The term pH stands for “potential of hydrogen,” which measures the concentration of hydrogen ions (H+) in a solution (e.g., urine).
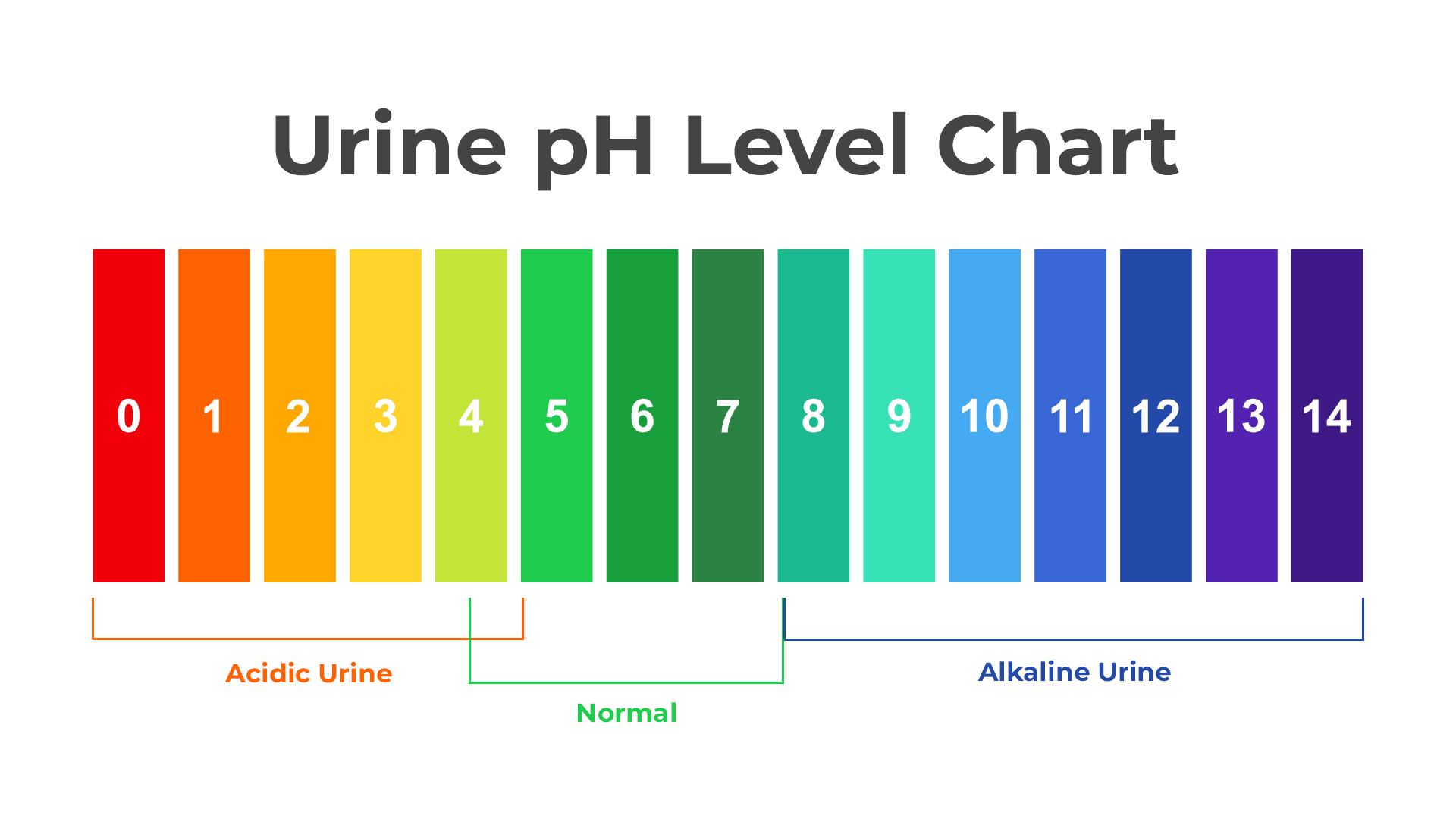
Ideally, urine should have a neutral pH level between 6.0 and 7.5. However, a slightly broader range (4.5 to 8.0) is generally acceptable. The pH scale ranges from 1 (highly acidic) to 14 (highly alkaline or basic).
Urine pH is a crucial risk factor to consider in terms of kidney stones. It directly impacts certain kidney stone types, such as calcium phosphate (CaP) and uric acid (UA) stones.
So, in this blog, we will dig deeper into urine pH’s role in kidney stone incidence. We will also discuss measures to keep it balanced to prevent kidney stones.
THE IMPORTANCE OF URINE PH
Urine pH provides valuable information about a person’s health. It is a potent indicator of many conditions around the urinary tract and metabolic health. For this reason, doctors frequently examine urine pH, together with other diagnostic tests.
Here are some reasons why a urine pH test is essential:
- Kidney Function: Urine pH can indicate how well the kidneys are functioning. Healthy kidneys help regulate the balance of acids and bases in the body, and changes in urine pH can be a sign of kidney problems.
- Metabolic Health: An abnormal pH level may be a clue that underlying metabolic disorders cause imbalances.
- Kidney stone risk: Monitoring urine pH can help identify individuals at risk of developing certain kidney stones.
- Urinary tract infection: Consistently alkaline urine may be associated with urinary tract infections.
- Medication Monitoring: Some medications can alter urine pH.
CAUSES OF ALKALINE AND ACIDIC URINE
Several things cause urine pH to become alkaline or acidic. We have to address these possible causes to ensure that our pH is optimal.
1. Diet
One of the critical factors that can influence urine pH is our diet. The foods we consume contribute to the alkalinity and acidity of our urine.
For instance, highly alkaline foods include:
- Most fruits
- Vegetables (especially leafy greens)
- Root vegetables (e.g., sweet potatoes and carrots)
- Nuts and Seeds
- Legumes
- Herbs and Spices (e.g., basil, parsley, and cilantro)
- Grains (e.g., quinoa, millet, and amaranth)
On the other hand, these are the foods that promote acidic urine:
- Refined grains (e.g., white bread and pasta)
- Processed foods
- Caffeinated beverages
- Sugary foods
- Sodas
- Alcoholic beverages
There had been a misconception regarding high-protein foods causing acidic urine. This is not true unless you have a metabolic dysfunction. A person with a healthy gut will not encounter this problem because meat, dairy, and other animal-based foods are efficiently digested and metabolized by humans.
2. Endogenous acid production (not due to diet)
Some researchers examined how factors like nutritional status and eating habits affect the amount of acid in the urine of people who form calcium-based kidney stones. Interestingly, their findings suggested that the primary reason for lower urinary pH levels in these individuals was the production of organic acids within the body rather than an acidic diet. Patients with high calcium or uric acid levels in their urine tended to have more organic acids and lower urinary pH.
However, experiments with mice lacking specific proteins involved in calcium handling (e.g., TRPV5 calcium channel) suggest otherwise. In this study, researchers reported that excessive calcium in the urine led to more alkaline urine pH.
Nevertheless, it’s important to note that this study is only retrospective (observational) and does not measure specific urinary components like sulfate (a marker of acid intake) or ammonium (an alkaline ion). Thus, more research is needed to fully understand these mechanisms in humans.
3. Metabolic acidosis
Metabolic acidosis is characterized by an excessive accumulation of acids or a loss of bicarbonate (a base) in the body due to impaired metabolic health. Bicarbonate is a crucial buffer in the body that helps counteract the effects of acids. This imbalance in the body’s acid-base regulation significantly affects urine pH.
If a person has this condition, urine pH becomes more acidic because the body attempts to eliminate excess acids from the bloodstream through the kidneys by excreting acidic hydrogen ions (H⁺) into the urine. As a result, the urine becomes more acidic to help balance the excess acidity in the body.
Nevertheless, when the body experiences metabolic acidosis, more phosphate is excreted in the urine. This happens because phosphate helps balance excess acidity. The intestines may absorb more phosphate, and the bones release phosphate, increasing urinary phosphate.
Meanwhile, the excretion of citrate in the urine is reduced. Citrate is a potent alkalizer that binds calcium in the urine, preventing the growth and aggregation of crystals. Excess acids in the blood will trigger increased citrate reabsorption in the kidney’s tubules, reducing its amounts in the urine.
Bicarbonate and ammonia (alkaline ions) are usually excreted in the urine too. However, conditions like insulin resistance and renal tubular acidosis (RTA) may hinder the kidneys from excreting enough of these ions to alkalize urine.
Acidosis also reduces the activity of the TRPV5 calcium channel in the kidneys (a calcium transporter), leading to increased urinary excretion of calcium and magnesium.
All these mechanisms raise the risk of kidney stone development.
4. Underlying conditions
Individuals who have type II diabetes have shown low levels of urinary ammonium (alkaline ion). This suggests that a lack of ammonia buffer might be responsible for the acidic urine and the likelihood of uric acid crystal formation.
The production of bicarbonate and ammonia in the kidney’s proximal tubule (the first segment of the functional unit) involves using glutamine (an amino acid). This process is stimulated when the body is in an acidic state (acidosis) and can also be regulated by insulin or glucocorticoids (a type of hormone).
The produced ammonium is then secreted into urine primarily through the sodium-hydrogen exchanger NHE3. Later, some ammonium is reabsorbed in the thick ascending limb of the loop of Henle (U-shaped structure) before being secreted into urine as ammonia (NH3) along the collecting duct. The final step of ammonia secretion into urine is facilitated by a protein called RhCG rhesus protein.
Research conducted on obese and diabetic rats and mice fed with high-calorie diets suggests that obesity and insulin resistance can affect the expression and activities of these transporters and enzymes. This leads to reduced ammonium excretion.
5. Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are typically due to bacteria in the urinary tract, like Escherichia coli (E. coli) and Proteus. These bacteria can produce ammonia as a metabolic byproduct. Ammonia production can raise urine pH. Severe UTI, then, can produce significant amounts of ammonia resulting in extremely alkaline urine.
6. Dehydration
When dehydrated, the body tries to conserve water by reducing urine output. The kidneys respond by concentrating the urine to retain as much water as possible. In concentrating urine, the kidneys actively reabsorb water and essential electrolytes (such as sodium) while leaving waste products and excess ions behind. This can result in a higher concentration of acidic waste products in the urine, leading to a lower pH (more acidic urine).
7. Medication
Some medications can alter urine pH as a side effect or as part of their intended therapeutic actions. Here are a few examples:
Acidifying Medications:
- Ammonium Chloride (used for metabolic conditions)
- Methenamine (an antibacterial)
Alkalinizing Medications:
- Potassium Citrate
- Sodium Bicarbonate
- Diuretics (e.g., Acetazolamide)
- Antacids (used for digestive issues)
URINE PH IMPACT ON KIDNEY STONES
The type of kidney stones that form in our bodies can be influenced by the acidity or alkalinity of our urine. When urine is more alkaline, it encourages the development of stones containing calcium and phosphate. On the other hand, if urine is more acidic, it promotes the formation of stones made of uric acid or cystine.
Calcium Phosphate Stones
Our body’s ability to handle substances like calcium, citrate, and phosphate is influenced by the pH level in our system. Several transport processes involving phosphate transporters, the citrate transporter NaDC1, and the TRPV5 calcium channel, are sensitive to changes in pH.
When urine pH exceeds 6, it significantly increases the likelihood of calcium phosphate (CaP) stones forming. CaP stones form when there are high calcium (hypercalciuria), and low citrate (hypocitraturia) levels in an alkaline urine environment.
Uric acid stones
As explained previously, people with obesity-related issues, like insulin resistance, may have low ammonium levels in their urine. That’s why they have more acidic urine and a higher chance of developing uric acid stones (UA).
The critical factor leading to the formation of uric acid stones in the kidneys is having a low urine pH level. Uric acid is a relatively weak organic acid with a property (pKa) around 5.5. When the urine’s pH is this low, it makes uric acid less soluble, causing crystals to form.
For instance, if someone has a urine pH of 5.3 and excretes about 800 mg of urate (a uric acid ion) per day, uric acid crystals are likely to form, even if daily urine volume is as high as two liters.
Calcium oxalate stones
Most calcium stones, which comprise about 80% of kidney stones, are primarily composed of a substance called calcium oxalate (CaOx). There has been a lot of debate regarding the role of urine pH in forming these stones. Most experts have found that calcium-oxalate stones can form regardless of the acidity or alkalinity of the urine. It’s unclear whether increasing urine pH (making it more alkaline) benefits CaOx stone-formers with low urine pH but normal urinary citrate levels.
Nevertheless, recent experimental research has revealed some intriguing findings. It showed that calcium oxalate in its monohydrate form (COM stones) crystallizes the most at 4.0 pH and least at 8.0 pH. This was confirmed through chemical analysis of the stones using Fourier-transform infrared spectroscopy (FTIR). Additionally, a laboratory technique called crystal-cell adhesion assay indicated that the crystals adhered most strongly to cells at the most acidic pH.

HOW TO TEST URINE PH?
A urine pH test is safe and doesn’t cause any side effects. You can check your urine pH either at home or at the hospital.
Doing it at home is very easy. You can simply use urine pH test strips, readily available at pharmacies or online. Just make sure to follow the instructions provided on the label for best results.
If you opt for a hospital test, the doctor may request a one-time urine sample or several samples within 24 hours. It’s essential to use the “clean-catch” method, where the person collects the midstream urine to ensure it’s free from external contaminants. You only need to collect about 2 oz. (60 milliliters) for pH testing.
Both one-time and 24-hour urine samples undergo a urinalysis, which consists of three main parts:
- Visual Examination: The doctor or lab technician visually inspects the color of the urine. They will also check for foreign materials like blood and assess whether it appears foamy.
- Chemical Dipstick Test: This test involves placing a specially treated paper (dipstick or litmus paper) into a urine sample. The dipstick changes color to indicate the acidity or alkalinity of the urine. It may also change color if other substances like glucose, white blood cells, bilirubin, or proteins are present.
- Microscopic Examination: A small portion of the urine is examined under a microscope to detect particles such as red blood cells, crystals, or white blood cells. These elements are not typically found in urine and can suggest underlying medical conditions.
CONCLUSION
Maintaining a neutral urine pH is essential for overall urinary health, and it can be achieved through certain dietary and lifestyle adjustments.
Metabolic dysfunction can often lead to imbalances in urine pH, so addressing this is essential. One effective strategy is shifting from plant-based to animal-based diets. Animal-based diets focus more on meat, organs, dairy, and fats than plant foods. Taking this route will cure your gut issues. Plus, animal products are 100% oxalate-free, meaning they are safe for kidney stone-formers. Nearly all plants contain oxalates and other harmful substances; that’s why they cause havoc inside our bodies.
There is still a lot more to learn about diet. So, if you want to dive deeper into the proper diet to prevent kidney stones and achieve overall health, check out our Coaching Program.
References




Interesting be good idea to check ones urine acidity.can be done easily at home if ya get the test strips.
Yes, it is good to test your urine pH regularly at home, especially if you form either calcium phosphate or uric acid stones.
Ty for response!
Thank YOU, @kats 🙂