Published: May 26, 2024 | 8 mins read
Distal Renal Tubular Acidosis Leads To Calcium Phosphate Stones
ARTICLE SHORTCUTS
- What is Distal Renal Tubular Acidosis?
- dRTA and Calcium Phosphate Stones
- Distal Renal Tubular Acidosis Causes
- Treat/Prevent dRTA and Calcium Phosphate Stones
One condition causes a snowball effect on calcium phosphate (CaP) stones. We are talking about distal renal tubular acidosis (dRTA). Does it ring a bell?
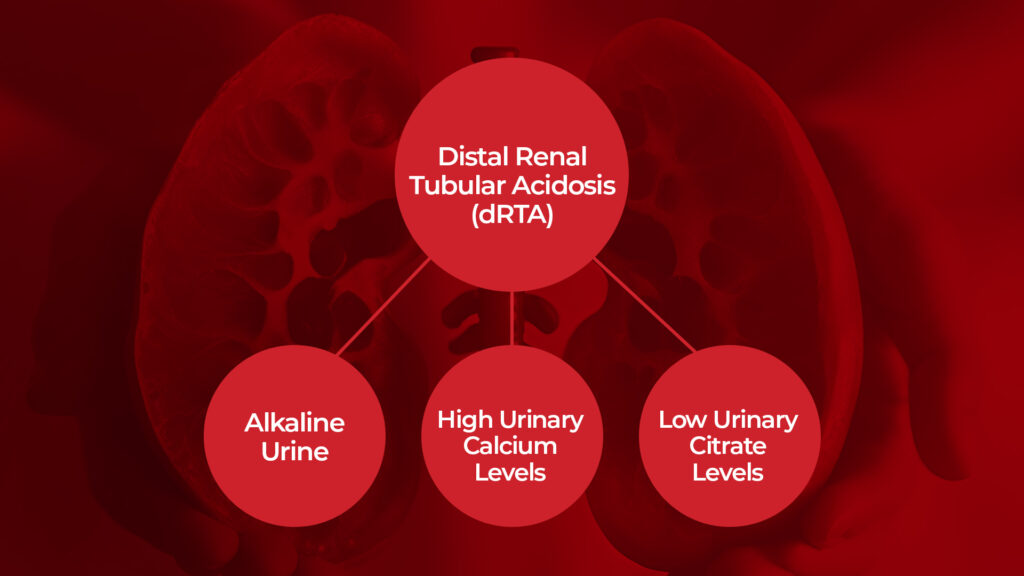
Diving into kidney stone research, we came across this critical topic. Distal renal tubular acidosis is a rare condition in which the kidneys can’t properly get rid of acid, leading to acid buildup in the blood. dRTA affects three major risk factors for CaP stones, which we will discuss in detail later.
In the meantime, let’s shed some light on what dRTA is about in the next section.
What is Distal Renal Tubular Acidosis?
Renal tubular acidosis (RTA) is when the kidneys don’t properly remove acids from the blood into the urine. This leads to high levels of acid in the blood, known as acidosis. This excess acid can disrupt various body functions. There are three main types:
- Type 1 (distal RTA) affects the end part of the kidney tubules.
- Type 2 (proximal RTA) affects the beginning part of the tubules.
- Type 4 (hyperkalemic RTA) happens when the kidneys struggle to remove enough potassium, impacting their acid-removing function.
You might wonder, “Why is there a Type 4 when there’s no Type 3?”
Well, type 3 RTA is less commonly used as a classification since it’s considered a mix of types 1 and 2.
In general, RTA is rare and often goes undiagnosed or misdiagnosed, making its exact frequency in the population unclear.
Anyway, in this blog, we will only focus on dRTA (Type 1) because this one is mainly connected to calcium phosphate stones among the three types.
That said, let’s proceed to the next section to better understand how distal renal tubular acidosis relates to this specific kidney stone type.
dRTA and Calcium Phosphate Stones
Most people suffering from distal renal tubular acidosis form calcium phosphate stones and calcium buildup in the kidneys (nephrocalcinosis). There are three main reasons why:
1. Alkaline urine (over 7.0 pH)
It is super frustrating when your kitchen sink gets clogged, and the dirty water from the dishes you washed doesn’t drain. This is kind of what happens with dRTA. The kidney tubules become dysfunctional, so they fail to excrete acid from the blood. As a result, acid imbalance occurs. The blood becomes acidic (acidemia), while the urine becomes alkaline.
Distal renal tubular acidosis causes alkaline urine because the kidneys are not excreting enough hydrogen ions (H+). Hydrogen ions are acidic, so the failure to excrete them in urine makes the urine alkaline.
Aside from alkalizing the urine, dRTA also lowers urinary citrate levels. Believe us, this is so troublesome if you are forming calcium stones. Read on to find out why.
2. Low citrate levels in the urine
To set the stage right, imagine citrate as Ironman’s armor. That’s what citrate‘s role is in this kidney stone movie. Citrate shields calcium by sticking to it to prevent stone-forming elements from doing so.
In other words, having low citrate levels is like Ironman going to war without his armor and weapons. GAME OVER!
But why do your citrate levels go low?
Your blood needs help buffering the acidity. Your mate needs the armor and the weapons, and you were too generous to lend them to him, even if that means you lose your battle like in a sad movie.
To add more conflict, dRTA increases another risk factor – urinary calcium.
3. Increased calcium levels in the urine
Because of the acid buildup, the body absorbs more calcium from food, releases more calcium from the bones, and reabsorbs less calcium in the kidney. This leads to high levels of calcium in the urine (hypercalciuria).
Well, calcium would not be problematic unless your urine is alkaline or you have other stone-forming elements waiting for a chance to bind to it (e.g., oxalates). If you’re not eating plant-based, calcium isn’t going to cause you kidney stones.
Okay, enough on the impact side. This time, let’s explore the possible causes of distal renal tubular acidosis to familiarize yourself with what you are dealing with.
Distal Renal Tubular Acidosis Causes
Distal renal tubular acidosis is pretty much like Jane Doe. You just don’t know precisely where dRTA came from. However, there are a couple of possible causes, which we have listed below.First, it can arise as a result of different autoimmune disorders that can impact various parts of the body, including the ability to remove acid from the blood:
- Sjögren’s syndrome – An autoimmune disease that commonly affects the joints and the moisture-producing glands in the body.
- Lupus – Affects multiple organs and systems in the body, including the skin, joints, kidneys, heart, and lungs.
- Rheumatoid arthritis – Affects the joints, causing inflammation, pain, stiffness, and swelling.
It can also result from congenital diseases (present at birth) but not hereditary, such as medullary sponge kidney (MSK), where tiny sacs form in kidney tissues, making it look like a sponge.
dRTA can also happen when you have cirrhosis, a chronic liver condition characterized by the gradual replacement of healthy liver tissue with scar tissue.
Furthermore, certain medications can trigger dRTA. These may include the following:
- Amphotericin B – An antifungal
- Lithium – A psychiatric medication
- Antibiotics (e.g., Pentamidine)
- Nonsteroidal Anti-inflammatory Drugs (e.g., Ibuprofen and Naproxen)
Individuals with inherited conditions like sickle cell anemia or Ehlers-Danlos syndrome might develop dRTA later on, too. In fact, researchers have found at least three genes that can contribute to dRTA:
- SLC4A1 gene – Mutations can impair bicarbonate transport, contributing to dRTA.
- ATP6V1B1 gene – Mutations can disrupt acid secretion, leading to dRTA.
- ATP6V0A4 gene – Mutations can impair acid secretion in the kidney, contributing to dRTA.
Did you know that people who have undergone kidney transplants may also develop distal renal tubular acidosis? This can be a result of rejection medications and specific injuries due to the procedure.
Suppose you have any of the conditions above that can lead to distal renal tubular acidosis and calcium phosphate stone risk. Is there a way for you to effectively manage this condition and lower your stone risk?
Of course! You can protect yourself! Find out how in the next section.
Treat/Prevent dRTA and Calcium Phosphate Stones
Distal renal tubular acidosis can be treated or at least managed. Your focus should be directed to the underlying cause if you can identify it exactly.
Suppose your dRTA isn’t genetic but instead due to an autoimmune disease. In that case, you can reverse it with the proper diet to boost your immunity. Remember, an autoimmune disease means your body attacks its healthy cells. It’s like a very drunk guy who punches you when you did nothing to deserve that blow. If this is your case, we invite you to our Coaching Program to learn the proper diet to fix your autoimmune condition and stop kidney stones.
Here’s a little secret. Congenital (present at birth) but not inherited issues like MSK are also related to diet. Our hypothesis is that calcium deficiency during pregnancy is driving this condition. So, pregnant moms should watch their calcium intake closely. If you want more details on this, we have a whole blog dedicated to MSK. The title is “Medullary Sponge Kidney Can Lead to Calcium Phosphate Stones!“
At the same time, you need to pay careful attention to preventing kidney stones. You need to increase your potassium and citrate intake through diet. Should you go with supplements? Nope. Our bodies treat synthetics as garbage, which is not really helpful. Aside from boosting potassium and citrate, we highly advise avoiding foods that will further increase your kidney stone risk (Ehem… plant foods)!
If you need help fixing your diet, join our Coaching Program today. We will assemble a plan to help you fix all the issues leading to distal renal tubular acidosis and kidney stones.
REFERENCE
1. Distal renal tubular acidosis: a systematic approach from diagnosis to treatment
2. Distal Renal Tubular Acidosis (dRTA): What is dRTA and how is it diagnosed?
3. Incomplete distal renal tubular acidosis and kidney stones
5. Renal tubular acidosis (RTA) and kidney stones: Diagnosis and management

Comments or questions?
Responses
WHAT TO READ NEXT
Publish Date: June 23, 2024
Do You Have a Phosphate Leak Leading to Kidney Stones?
Publish Date: June 9, 2024
The #1 Genetic Cause Of Kidney Stones: Cystinuria Disease
Publish Date: May 19, 2024
Medullary Sponge Kidney Can Lead to Calcium Phosphate Stones!