Published: March 28, 2022 | 17 mins read
American Urological Association (AUA) Guidelines for the Treatment of Kidney Stones
Kidney stones are a common and costly disease affecting roughly 15% of the global population and rising. Direct and indirect treatment costs have been estimated in the several billions of dollars per year. The treatment of kidney stones can be complex and there are numerous competing techniques that may be used. Proper treatment selection is the greatest predictor of a successful outcome. As such, the American Urological Association (AUA) has compiled guidelines based on observational studies from around the globe to provide Urologists and patients with the best care possible.

DIAGNOSIS
Most individuals learn of their kidney stones when a massive wave a pain hits them from out of nowhere. This pain typically leads to a trip to the ER where imaging is performed in an attempt to identify the source of the pain. There are many options available for imaging. However, if this is your first kidney stone, the American Urological Association (AUA) recommends non-contrast computed tomography (NCCT). The AUA recommends CT over all other imaging options due to it’s high degree of accuracy in identify stones. Additionally, stone density can be obtained from this imaging modality that can be used later when considering treatment option.
Ultrasound has become more popular over time due to it’s low cost. However, it is much less accurate in identifying stones when compared to CT. Again, if this is your first kidney stone, you should ask/receive a CT scan. However, for future kidney stones, Ultrasound may be used as kidney stone types rarely change over time and you will have obtained what you need to know from your initial CT scan.
For more information on the imaging options currently in use, please read our Kidney Stone Imaging Techniques blog.
According to the American Urological Association (AUA), doctors are required to obtain a urinalysis prior to any intervention (surgical or otherwise). However, based on personal experience and thousands of interactions with individuals across the globe, this might take place 20% of the time. And, that’s being generous!
Obtaining a urinalysis is critical in order to minimize the risks of infectious complications. Fortunately, infection stones or infections related to stones are relatively rare. But, if the culture comes back positive for infection, this will need to be treated with antibiotics to sterilize the urine before any intervention, surgical or otherwise, should be attempted.
While many of you, including myself, are not fans of antibiotic use. It is warranted in this application due to the risk of severe complications that infections can cause if left untreated such as sepsis, kidney failure, and death. It’s no joke!
So, if you’re walking out the door of the ER, hospital, or Urologist/Doctors office without this. Turn right back around and get this done!
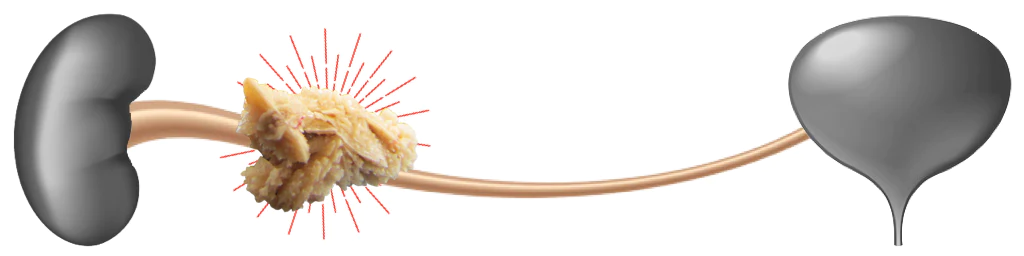
STONES IN URETER
Uncomplicated Stones < 10mm
Studies have shown that the likelihood of spontaneous stone passage correlated with stone size and location. The smaller the stone and the lower down its location in the urinary tract, the greater the possibility of spontaneous passage. Additionally, smaller stones are likely to pass more quickly than larger stones.
In a review of several Randomized Control Studies evaluating the efficacy of Expulsive Therapy, roughly half of the patients with lower urinary tract stones spontaneously passed their stones without any other intervention. As such, the AUA has found ample evidence to suggest that passage of stones located in the ureter of less than 10mm is possible for individuals with well-controlled pain, no signs of infection, or high grade obstruction (hydronephrosis).
Uncomplicated: well-controlled pain, no signs of infection, or high grade obstruction (hydronephrosis)
To learn more about Expulsive Therapy, please read our Expulsive Therapy for Kidney Stones blog.
Failed Expulsive Therapy
According to the American Urological Association (AUA), Ureteroscopy (URS) has higher stone-free rates in a single procedure when compared to Shockwave Lithotripsy (SWL) for stones in the ureter. This disparity was more prominent in stones less than 10mm located in the mid to lower ureter. Therefore, URS is recommended as the first-line treatment and SWL is offered as an acceptable alternative.
It is important to note that stone-free rates are higher for Ureteroscopy (URS) than with Shockwave Lithotripsy (SWL) at all locations in the ureter. Additionally, URS is more successful in achieving a complete stone-free status after a single session. However, URS has a higher rate of complications. There’s always a trade-off!
Cystine or Uric Acid Stones
For individuals with known or suspected Cystinuria or uric acid kidney stones, choosing the correct treatment can be complex. Cystine stones are often only faintly visible on x-ray (radiopaque) and pure uric acid stones are not visible on x-ray (radiolucent). As such, stone targeting during Shockwave Lithotripsy (SWL) with Fluoroscopy will be challenging if not impossible. Additionally, the more dense version of cystine stones are resistant to SWL fragmentation. Thus, Ureteroscopy (URS) is the recommended first-line treatment option.
NOTE: The American Urological Association (AUA) is only concerned with surgical and pharmaceutical interventions. They do not research or make comment regarding naturopathic approaches to the management of kidney stones. A natural expulsive such as our product, CLEANSE, can very quickly dissolve and pass both cystine and uric acid kidney stones negating the need for URS or SWL.
Failed SWL/URS
In some individuals with large or complex stones in the ureter, neither Shockwave Lithotripsy (SWL) nor Ureteroscopy (URS) are likely to attain the desired stone-free rate after a reasonable number of sessions. In cases such as these, Percutaneous Nephrolithotomy (PCNL) may allow for faster stone removal.

STONES IN KIDNEY
Symptomatic Non-Lower Pole Stones < 20mm
Treatment options for individuals with non-lower pole stones less than 20mm include Shockwave Lithotripsy (SWL), Ureteroscopy (URS), and Percutaneous Nephrolithotomy (PCNL). Stone-free rates using PCNL are the least affected by stone size, while stone-free rates of both SWL and URS decrease as stone size increases. However, for stones less than 20mm, stone-free rates for both SWL and URS are acceptable and have less complications than PCNL.
Of the two options (URS and SWL), URS is associated with higher success rates in a single procedure. Therefore, the patient will become stone-free faster than with SWL.
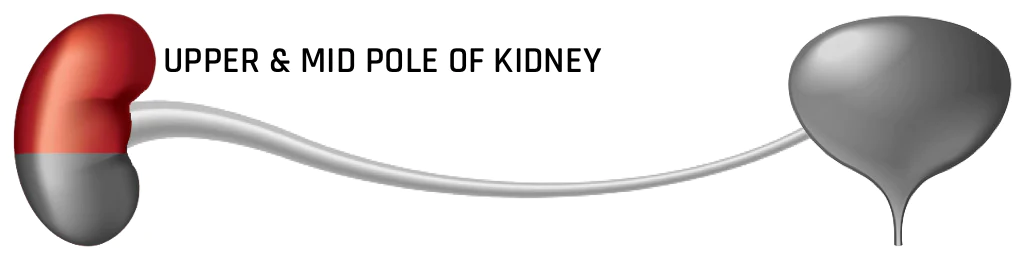
Symptomatic Non- Lower Pole Stone > 20mm
Percutaneous Nephrolithotomy (PCNL) should is recommended as first-line treatment for individuals with stones larger than 20mm. This is due to the higher stone-free rate of PCNL compared to Shockwave Lithotripsy (SWL) or Ureteroscopy (URS). Additionally PCNL is less invasive than open surgery or laparoscopic procedures. Compared to SWL and URS, PCNL is also less affected by stone composition, density, and location. However, the benefit of higher stone-free rates must be weighed against the increased invasiveness and risk for complication with PCNL.
The American Urological Association (AUA) has also made a note to point out that In patients with stones > 20mm should not be offered SWL as first-line treatment. SWL is often considered an attractive treatment option by patients and Urologists due to its minimally invasive nature and lower complication rates when compared to PCNL and URS. However, with large stones, SWL oftentimes requires multiple procedures and has lower stone-free rates. With large stones there is also risk that the fragments could cause an obstruction leading to further complications.
Staghorn Stones
According to the American Urological Association (AUA), Percutaneous Nephrolithotomy (PCNL) should be the first line treatment choice for staghorn kidney stones. PCNL offers a lower rate of complications, decreased hospital stay time, and earlier return to work when compared to more traditional open surgeries which are less and less used today. PCNL has also been shown to have three times higher stone-free rates compared to Shockwave Lithotripsy (SWL).
Asymptomatic/Non-Obstructing Stones
The detection of asymptomatic (no symptoms) stones has increased in recent years. This has largely been filed by the increased use of CT imaging. According to the American Urological Association (AUA), observation of asymptomatic, non-obstructing stones is appropriate as long as the individual is counseled regarding the risks of stone growth, passage, and pain.
However, there are certain situations for which treatment of asymptomatic, non-obstructing stones is more appropriate than observation. Treatment should be considered in cases associated with infection or for vocational reasons (ex: airline pilots or military personnel).
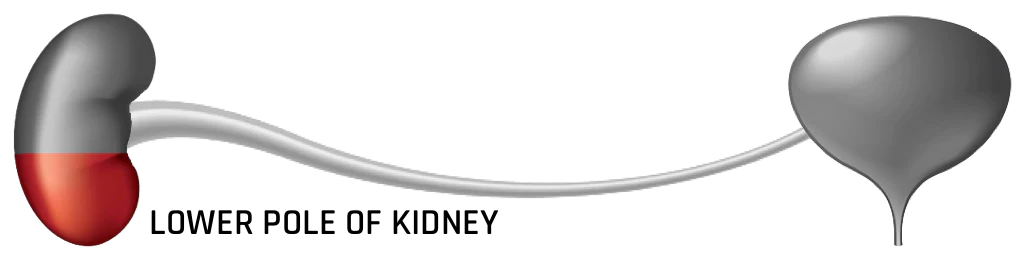
Symptomatic Lower Pole Stones < 10mm
In the treatment of lower pole kidney stones, there was no statistically significant data to differentiate between Ureterocscopy (URS) or Shockwave Lithotripsy (SWL). Complications during surgery have been shown to be somewhat higher with URS. Quality of life for the patient has also been shown to be higher with SWL.
NOTE: Individuals with skin-to-stone distance greater than 9-10cm or stone density greater than 1000HU will have less successful results with SWL.
Lower Pole Stone Stones > 10mm
Treatment options for lower pole kidney stones greater than 10mm are Percutaneous Nephrolithotomy (PCNL), Ureteroscopy (URS), or Shockwave Lithotripsy (SWL). Randomized trials have demonstrated that PCNL has superior single treatment stone-free rates. However this comes at the cost of higher rates of complications. While URS and SWL are options for the management of these stones, re-treatment rates are higher, stone-free rates are significantly lower, and there is a higher likelihood of stone recurrence due to retained fragments after the procedures.
As such, PCNL should be considered the primary treatment for most instances. However, individuals must be well-briefed on the nature of the procedure and expected complications. PCNL performed with smaller access tracts (“Miniperc” or “Microperc”) may allow for similar outcomes with lower complication rates.
Non-PCNL Candidates
While Percutaneous Nephrolithotomy (PCNL) is the optimal treatment for patients with complex, large (> 20mm), and staghorn stones, some anatomic abnormalities and/or patient-related factors may prove difficult under this treatment modality. Individuals who are on anti-coagulation or anti-platelet therapy that cannot be discontinued or those with the presence of contractures, flexion deformities, or other anatomical derangements that may make patient positioning challenging or impossible.
In these situations, Ureteroscopy (URS) is a viable option. However, it may require multiple staged procedures to treat large stones and may not leave the individual completely stone-free. URS can safely be performed in patients undergoing anti-coagulation or anti-platelet therapy.
Symptomatic Calyceal Diverticular Stones
The stone-free rates achieved with Shockwave Lithotripsy (SWL) for treating individuals with calyceal diverticular stones are very low (0-25%). While SWL may be able to reduce the size of their stone, there is risk for recurrence or new stone growth.
Substantially higher stone-free rates are attainable using Ureteroscopy (URS) or Percutaneous Nephrolithotomy (PCNL). Ultimately, the choice to use URS or PCNL should be based on stone location, size, surrounding anatomical structures, and patient preference.

TREATMENT OF PEDIATRIC PATIENTS
Uncomplicated Ureteral Stones < 10mm
The American Urological Association (AUA) recommends an initial trial of observation with or without Expulsive Therapy. Studies have shown that a significant proportion of children will pass their stones spontaneously; avoiding the need for surgical intervention. However, as stone size increased towards 1cm, the rate of spontaneous passage decreased.
Failed Expulsive Therapy
In children who are unlikely to pass their ureteral stone spontaneously or have failed Expulsive Therapy, surgical intervention using either Shockwave Lithotripsy (SWL) or Ureteroscopy (URS) to treat the stone is appropriate.
Stones in Kidney < 20mm
Shockwave Lithotripsy (SWL) has a long track record of success in the treatment of kidney stones in children. Stone-free rates are relatively high (80-85% overall). Complication rates are also low with very little evidence of any long-term consequences to the procedure.
Ureteroscopy (URS) also has a high rate of success in children with stone-free rates of around 85%. However, complication rates may be higher with URS (12.4%-20.5%)
Stones in Kidney > 20mm
High stone-free rates have been reported with both Percutaneous Nephrolithotomy (PCNL) and Shockwave Lithotripsy (SWL) in children with larger kidney stones. SWL has stone-free rates of 73%-83% while PCNL stone-free rates approach 90%. If SWL is performed, the child must endure the placement of a ureteral stent or nephrostomy tube (drains urine directly from kidney into external bladder) to prevent post-operative obstructions due to stone fragments.
Several factors must be evaluated when selecting the most appropriate procedure to use including:
- Stone composition
- Stone density
- Stone location
- Child’s physical build
- Kidney collecting system anatomy
- Relation of kidney to surrounding tissues
- Potential medical complications
- Parental preference
Asymptomatic Non-Obstructing Stones in Kidney
While observation of asymptomatic, non-obstructing kidney stones is an option for children, these patients should be seen regularly to monitor stones for increases in size or additional stones. Metabolic evaluation for stone risk factors should also be conducted as the incidence of metabolic abnormalities is high in children who form kidney stones. Twenty-four hour urine collections are appropriate in toilet-trained children and “spot” urine samples can still be used to screen for hypercalciuria. Infants and young children with Hyperoxaluria should be screened for Primary Hyperoxaluria.
- Hypercalciuria: excess calcium in the urine
- Hyperoxaluria: excess oxalate (oxalic acid) in the urine

TREATMENT OF PREGNANT PATIENTS
Stone in Ureter (Controlled Symptoms)
The spontaneous passage rate for pregnant women with stones located in the ureter is no different than the rest of the population. Therefore, in patients whose symptoms are uncomplicated, a period of observation is the recommended first step. It is important to note that a stone-related event does carry with it an increased risk of maternal and fetal complications. As such, patients need to be closely followed for recurrent or persistent symptoms.
If Medical Expulsive Therapy (MET) is considered, it is important to note that this approach has not been well investigated in the pregnant population. There are studies that show MET to be safe during the 2nd or 3rd trimesters. But, additional research is needed.
NOTE: NSAIDs like aspirin, Ibuprofen, Advil, and Ketorolac are contraindicated during pregnancy and should not be taken.
Failed Observation
If observation fails for the pregnant patient, it may become necessary to intervene. The use of a ureteral stent or a percutaneous nephrostomoy tube (puncture made into your side and into kidney where tube is inserted to drain urine) will both effectively relieve the kidney from stress due to a back-up of urine. However, the introduction of foreign objects like this into the kidney of a pregnant woman is concerning as they have a tendency to become encrusted rapidly.
As an alternative, Ureteroscopy (URS) can be used to achieve high stone free rates. However, URS in pregnant patients should only be untaken by Urologists familiar with the treatment approach and at an institution that has both the equipment and obstetric support for maternal and fetal safety.

STENTS
Patients Undergoing Shockwave Lithotripsy (SWL)
Some patients with stones located in the ureter will have a stent placed to relieve pain and allow free flow of urine until surgery can be performed. However, some Urologists place uterus stents prior to Shockwave Lithotripsy (SWL) in an effort to improve the stone-free rate or prevent complications. Both the American Urological Association (AUA) and European Association of Urology (EAU) recommend against routine stent use with SWL based on comparable stone-free rates with or without the use of a stent.
Pre-Ureteroscopy (URS)
Some patients undergoing Ureteroscopy (URS) to treat a stone in their ureter will have a stent placed prior to the procedure to relive pain and/or obstruction. Recently, Urologists have started to place stents prior to URS with the intention of dilating the ureter and improving stone-free rates. Stent us prior to URS has been shown to reduce operative time and reduce the need for additional operations in patients with stones less than 10mm.
However, the American Urological Association (AUA) recommends against routine stent placement prior to Ureteroscopy (URS) when the sole purpose is to increase stone-free rates or reduce operative time. The rationale for this is that the improved stone-free rates do not override the added care costs and negative impact on quality of life for the patient associated with stent use.
Following Ureteroscopy (URS) Procedure
The insertion of a ureteral stent has long been considered routine practice after Ureteroscopy (URS). However, provided that your URS was performed successfully, the use of a stent post-operatively is not required. To be defined as successful, patients must meet the following criteria to avoid stent placement:
- No suspected injury to the ureter
- No abnormal narrowing in the ureter (ureteral strictures)
- No other anatomical impediments to stone fragment passage
- Normal contralateral kidney (two kidneys)
- No renal functional impairments
- No secondary URS procedure is planned
Obstructing Stone or Suspected Infection
Stone manipulation in the setting of an active, untreated infection with an associated urinary tract obstruction (from a kidney stone) can lead to life threatening sepsis. In this situation, it is mandated that the kidney be drained either with a nephrostomy tube or ureteral stent to allow drainage of the infected urine and to permit antibiotic penetration into the affected kidney. The rate of mortality doubles when drainage is not performed.
The choice of drainage technique (stent or nephrostomy tube) is left at the discretion of the Urologist. Both are equally effective. However, the nephrostomy tube is more invasive as it requires a puncture into the patient’s side and kidney, which comes with an associated increase in the risk of complications.
Stent Discomfort
It’s no secret. Stents are incredibly uncomfortable. Fortunately, alpha-blockers may be prescribed to help reduce stent-related discomfort. Other medication that can be used include:
- Anticholinergics (block action of acetylcholine which is a neurotransmitter that transfers signals between certain cells to affect how your body functions)
- Antimuscarinics (treats overactive bladder)
- Bladder analgesics for dysuria (pain medication)
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Narcotic Analgesics
Pediatric Patients
In children who require Ureteroscopy (URS) to treat a stone in their ureter, access is sometimes difficult due to their narrow ureterovesical junction and/or ureter. In adult patients, placement of a ureteral stent typically results in passive dilation (expansion) of the ureter, thus permitting better access to the kidney. However, “pre-stenting” in children should not be considered a routine practice since access to the upper urinary tract is possible on the initial attempt in a majority of children undergoing URS.

POST PASSAGE
Once you have either successfully passed your stone whole, in fragments, or as “sand” collected in your urine strainer (you’re straining your urine, right?), it is imperative that you bring your stone/remnants to your Urologist for analysis. The chemical analysis will report back the specific composition of your stone type. Once the stone type has been identified, steps can be taken to prevent future kidney stones for most of the major stone types.
The only exception to this would be if you have already had a previous kidney stone analyzed. Stone composition rarely changes unless major dietary and/or lifestyle changes have been made.
This is considered to be a “Clinical Principle” by the American Urological Association (AUA) and should not be ignored. Unfortunately, this is a step that is skipped roughly 95% of the time based on the tens of thousands of kidney stones sufferers that we have engaged with over the last 4 years.
You, and only you, are responsible for your health! So, speak up when something doesn’t sound right or is missed (like getting your stone analyzed) ????
References

Comments or questions?
Responses
WHAT TO READ NEXT
Publish Date: December 3, 2023
The Stent Survival Guide
Publish Date: March 20, 2022
Percutaneous Nephrolithotomy (PCNL) for Kidney Stones
Publish Date: February 20, 2022
Ureteroscopy for the Treatment of Kidney Stones