Published: December 3, 2023 | 5 mins read
The Stent Survival Guide
The use of stents for kidney stones is on the rise. But are they necessary?
More importantly, how does a stent feel once it’s in place?
Well, you came to the right place!
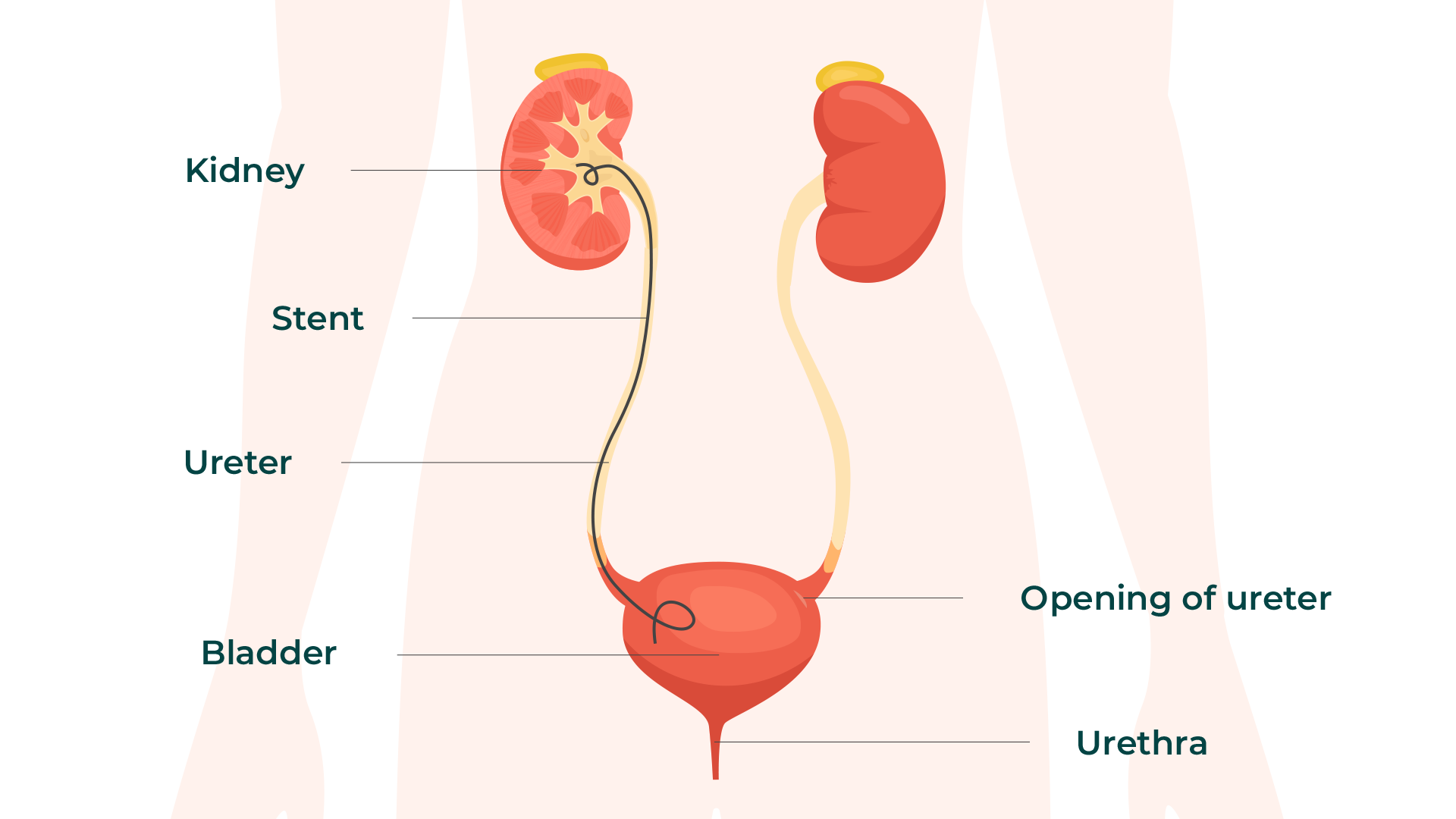
First, let’s define what a stent is. Basically, it’s just a thin, long tube placed inside your urinary tract.
The primary purpose of a stent is to drain the urine that gets stuck in your kidneys because something is obstructing its flow. It could be a kidney stone (the most common reason) or something else.
DO YOU NEED A STENT?
Not all the time.
For example, the American Urological Association (AUA) doesn’t advise routine stenting for Shock Wave Lithotripsy patients. That’s because stents do not improve stone-free rates at all.
The sole job of stents is to relieve pressure from a back-up of urine in the kidneys.
The AUA also discourages placing a ureteral stent before or after Ureteroscopy unless you meet these criteria:
- Suspected injury to the ureter during Ureteroscopy
- There is evidence of blockages or obstructions because of stone fragments.
- The kidney on the opposite side is not working normally.
- There is kidney function impairment.
- A second Ureteroscopy procedure is needed.
If you DON’T meet these criteria, YOU DON’T NEED A STENT. And it’s OK to tell your doctor this!
One point of confusion with stents is that people are led to believe that the stent will increase the speed of stone passage or improve the odds of their stone passing. However, this is not the case.
Stents stop the progress of your stone passage!
Plus, you’ll be saddled with all the discomfort from the stent and the additional medical bills accompanying them.
Stenting is only advised in the presence of a severe infection or an obstruction that leads to elevated grades of hydronephrosis, where the urine needs to be drained immediately.
WHAT TO EXPECT DURING INSERTION
Stent insertion is NOT a cloud nine experience. So before the procedure, you’ll be given either general or local anesthesia to help make this a little easier.
Sedation may help if you are scared or anxious. But it won’t do much for the pain.
Sedative drugs, including propofol, benzodiazepine, dexmedetomidine, and ketamine, are commonly used. However, you’ll remain awake and responsive.
For pain reduction, opioids are another option. But proper assistance is required regarding usage and dosage to avoid risks. Examples can include codeine, morphine, oxycodone, and hydrocodone.
HOW DOES A STENT FEEL?
The discomfort will begin right after the anesthesia or pain reliever wears off. This is for sure!
Expect to experience burning urination for the first 72 hours after a ureteral stent is put in place.
Unfortunately, stents are just a pain, with around 80 percent of people stating discomfort as a significant issue.
Sadly, the discomfort will not leave you until the stent has been removed. Here’s a snapshot of what you might experience:
- Bladder spasms (discomfort or pain after urination)
- Frequent urination
- Bladder irritation with a strong urge to urinate
- Ureteral Reflux (urine back-flowing into the ureter, causing pain)
- Flank/Abdominal Pain (similar to a full bladder)
- Blood in the urine

MANAGING PAIN & DISCOMFORT
Regardless of what kind of stent you have, the pain and discomfort are almost the same. However, given the length of time that you have the stent in place, here are a few options to lessen your trouble:
For burning urination:
- “Phenazopyridine” (Pyridium or AZO)
- Proper hydration with 96-128oz water daily
For bladder spasms and frequent urination:
- Alpha-blocker class drug (Ex. Tamsulosin and Alfuzosin)
- Anticholinergics (Ex. Ditropan and Detrol)
- Natural remedies like marshmallow root, horsetail and chamomile (which are also low in oxalates)
For pain:
- NSAIDs (Ex. Ibuprofen and naproxen)
- Opioids
- Natural remedies like dandelion root, marshmallow root, and chanca piedra (which are also helpful if you are battling kidney stones).
HOW LONG ARE STENTS KEPT IN PLACE?
According to the AUA, the duration of ureteral stenting after stone removal should be around three to seven days. Especially if there’s no compelling reason (like severe swelling) to keep it longer. Because again, the sole reason you need it is to drain your stuck urine. Plus, the longer you have it, the longer you suffer from discomfort.
Also, the shorter the time you have the stent in, the lesser the chance of stent-related complications like UTIs and encrustation.
It could be longer, though, depending on the need. However, it is essential to remember to have it replaced within three months.
Replacing the stent every three months helps to prevent infection and encrustation. Encrustation means forming a crystal coating from bacterial buildup, which can be almost as bad as kidney stones!
If a stent is left in place for over 12 weeks, it is 76% likely to develop encrustation. This will cause further blockage of the ureter and more pain.
If you have more questions about ureteral stents, contact us or join our Coaching Program to receive all the support you need.




Based on an ultra sound I have slightly enlarged prostrate and am retaining some urine. My urologist hasn’t pushed stents, but has suggested it might be necessary down the road. Do you have any suggestions to naturally cure one or both conditions. I subscribe to your supplement and take it every day.
Hey Allen,
Great question! When it comes to prostate issues, we actually have a blog and video that will be coming out in the very near future on this exact subject 🙂
But we won’t make you wait!
Enlarged prostate issues are almost always tied to insulin problems. Insulin controls glucose levels in the blood and is like Miracle Grow for your prostate (and it gets more and more potent as men age).
Any insulin-related problem is always tied to the foods you eat (unless you’ve got Type 1 Diabetes). So, we’d encourage you to investigate the foods you’re eating to look for things with added sugar (like high fructose corn syrup or even just regular table sugar) and high carbohydrates. These are typically the easiest to spot and fix.
Then, there’s the issue of consuming too little animal protein. If you don’t consume enough animal protein, your body’s ability to regulate insulin goes haywire. And prostate issues can result in men.
This is where we’d suggest that you start!
We hope this helps 🙂
– The Stone Relief Team
Shoot us all your questions about stents!