Published: February 20, 2022 | 39 mins read
Ureteroscopy for the Treatment of Kidney Stones
Ureteroscopy has evolved to be one of the primary treatment options for kidney stones since its introduction in 1964. The advancement in laser technology has largely fueled the growth of this kidney stone treatment method, which is net positive for all involved as ureteroscopic treatment is most commonly used to manage obstructive and/or large kidney stones.
Before we dive into this topic more, let’s get a few definitions out of the way to help better understand the different procedural options within this treatment modality.
WHAT IS URETEROSCOPY?
Ureteroscopy is defined as a procedure in which a small scope (the ureteroscope) is inserted into the urinary tract. Second, Ureteroscoy is ultimately part of a larger family of surgical procedures called Endoscopy. Endoscopy is a general reference to any technique utilizing an instrument inserted into the body to provide a view of its internal parts. Lastly, the word lithotripsy gets thrown around often and is frequently inappropriately associated with a specific procedure. Lithotripsy is any procedure involving the physical destruction of hardened masses (like kidney stones) to set the record straight. The term is derived from the Greek words meaning “breaking stones.”

Additionally, let’s take a moment to differentiate between intracorporeal and extracorporeal. Anything with an “intra” pre-fix refers to work being conducted inside the body (ex: RIRS “Retrograde Intrarenal Surgery” = ureteroscopic procedure performed inside the body). Anything with the “extra” pre-fix related to work conducted outside the body (ex: Extracorporeal Shockwave Lithotripsy = shockwave lithotripsy applied from outside of the body).
Ok, with that out of the way, we can move forward ????
AMERICAN UROLOGICAL ASSOCIATION PATIENT SELECTION CRITERIA
In the treatment of adult patients with ureteral stones:
- Patients with uncomplicated ureteral stones <10 mm should be offered observation, and those with distal stones of similar size should be offered Expulsive Therapy (ET).
- Clinicians should inform patients that Shockwave Lithotripsy (SWL) is the procedure with the least morbidity and lowest complication rate, but Ureteroscopy (URS) has a greater stone-free rate in a single procedure.
- In patients with mid or distal ureteral stones who require intervention (who were not candidates for or who failed Expulsive Therapy-ET), clinicians should recommend Ureteroscopy (URS) as first-line therapy. For patients who decline URS, clinicians should offer Shockwave Lithotripsy (SWL).
- Ureteroscopy (URS) is recommended for patients with suspected cystine or uric acid ureteral stones who fail Expulsive Therapy (ET) or desire intervention.
In the treatment of adult patients with renal stones (stones still in the kidney):
- In symptomatic patients with a total non-lower pole renal stone burden ≤ 20mm, clinicians may offer Shockwave Lithotripsy (SWL) or Ureteroscopy (URS).
- Clinicians should offer Shockwave Lithotripsy (SWL) or Ureteroscopy (URS) to patients with symptomatic ≤ 10mm lower pole renal stones.
- In patients not considered candidates for Percutaneous Nephrolithotomy (PCNL), clinicians may offer staged Ureteroscopy (URS).
- In patients with symptomatic calyceal diverticular stones, endoscopic therapy (Ureteroscopy- URS, Percutaneous Nephrolithotomy- PCNL, laparoscopic, robotic) should be preferentially utilized.
In the treatment of pregnant patients with ureteral or renal stones:
- In pregnant patients with ureteral stones, clinicians may offer Ureteroscopy (URS) to patients who fail observation. Ureteral stent and nephrostomy tube are alternative options with frequent stent or tube changes usually being necessary.
General Recommendations for all patients with ureteral or renal stones:
- Clinicians should use Ureteroscopy (URS) as first-line therapy in most patients who require stone intervention in the setting of uncorrected bleeding diatheses or who require continuous anticoagulation/anti-platelet therapy.
PRE-OPERATIVE CONSIDERATIONS
Determining whether a patient is a candidate for Ureteroscopy would be the first step in maximizing stone-free rates. Multiple pre-operative predictors have been suggested below as tools to improve decision-making and better counsel patients on anticipated outcomes. The American Urological Association recommends a non-contrast CT scan to help select the best candidates and evaluate parameters that will impact success rates. The parameters that will require evaluation by your Urologist are as follows:
- Stone burden (total volume of all stones in system)
- Hydronephrosis severity (None-Mild-Moderate-Severe)
- Stone location
- Number of stones
- Computed Tomography (CT) stone attenuation
- Age
- Sex
- Pre-operative Stenting
- Pre-operative alpha-blockers
- Surgeon volume
The most influential parameters are consistently stone burden and location.
STENTS
Pre-stenting improves the stone-free rate and reduces intro-operative complications. Additionally, pre-stenting positively affects the safety and efficacy of Ureteroscopic procedures. It can also facilitate access to the ureteroscope and access sheath.
ALPHA-BLOCKERS
As discussed in previous blogs, the Alpha-Blocker drug class plays a role in Medical Expulsive Therapy (ET). This is primarily due to the urinary tract being lined with adrenergic receptors in varying density for which this drug class acts.
There are three subtypes of alpha-1 adrenoceptors (ARs) in the ureteric wall: alpha-1A, alpha-1B, and alpha-1D. In the proximal (upper) ureter, the distribution of these adrenoreceptors is alpha-1D ≥ alpha-1B > alpha-1A. In the distal (lower) and mid ureter, the distribution of Ads is alpha-1D > alpha-1A > alpha-1B.
Flo-max, the most commonly prescribed alpha-blocker, acts on alpha-1A and alpha-1D receptors, causing the relaxation of the ureteric wall. This increases the urine bolus and intra-ureteral pressure above the stone while lowering intra-ureteral pressure below the stone by decreasing peristalsis, thus increasing stone expulsion.
NOTE: in the Natural Expulsive Therapy setting, a combination of antispasmodics, anti-inflammatories, and diuretics are used to accomplish this identical mechanism as within Medical Expulsive Therapy.
The application of pre-operative Flo-max has been suggested to decrease the need for pre-operative ureteric dilation and increase the procedure’s success rate. Let’s look at the results from a 2020 study conducted in Egypt investigating the impact of pre-operative use of alpha-blockers before Ureteroscopy.
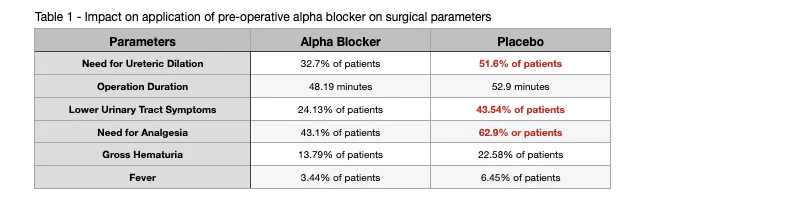
As you can see by the data represented in Table 1 above, pre-operative alpha-blockers such as Flo-max significantly decrease the need for intra-operative dilation. Additionally, it leads to a significant decrease in the development of post-operative lower urinary tract symptoms, post-operative pain, and the need for analgesics.
PREVIOUS OPEN OR PERCUTANEOUS SURGERY
Open or percutaneous surgery for kidney stones can harm the kidney’s collecting system. As such, Retrograde Intrarenal Surgery (RIRS) has been proposed as an alternative to Percutaneous Nephrolithotomy (PCNL) and Shockwave Lithotripsy (SWL) due to its high stone-free rates and the low number of reported complications.
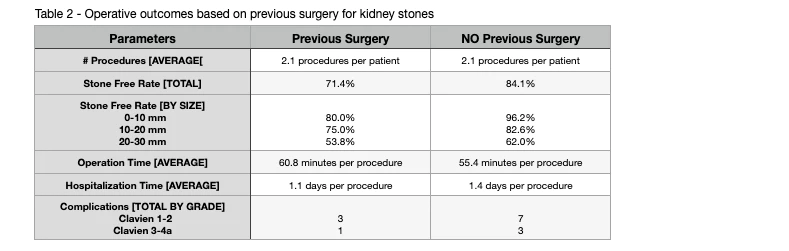
As you can see from Table 2 above, individuals who had previous open or percutaneous surgeries had lower stone-free rates after the procedure. This can be attributed to the impaired renal anatomy of earlier surgeries, making it challenging to access stones. In addition, the spontaneous stone passage of residual fragments is negatively affected for those with previous surgeries.
MEDICATIONS TO AVOID
Ureteroscopy is the only minimally-invasive stone surgery performed while on active anti-coagulation. Even with this option, it is preferable to discontinue all blood thinners before surgery, if medically possible. Please contact your surgeon’s office if you are unsure which medications to stop before surgery. The following is a list of medications to avoid at least 7-10 days before surgery. Many of these medications can alter platelet function or your body’s ability to clot, which may contribute to unwanted bleeding during or after surgery. Do not stop any medicine without contacting the prescribing doctor to get their approval.
- Aspirin, Motrin, Ibuprofen, Advil, Alka Seltzer, Vitamin E, Ticlid, Coumadin, Lovenox, Celebrex, Voltaren, Vioxx, Plavix
- A formal list of these medications and others will be provided to you by our Surgery Scheduling Coordinators.
There is no bowel preparation needed for ureteroscopy. However, most patients are asked to be NPO (“nothing by mouth”) after midnight of the night before surgery.
ANESTHESIA
Routinely, most urologists prefer general anesthesia (GA) during surgery for kidney stones. Under general anesthesia, the patient’s breathing and movement can be controlled, allowing the increased patient and surgeon comfort. However, some studies suggest that mortality and significant complications can be reduced through regional anesthesia applied through the spine. Although spinal anesthesia may be preferred in critically ill patients, there is no difference in major outcomes or critical complications between general anesthesia and regional-spinal anesthesia. Therefore, these two anesthesia methods are suitable for Ureteroscopy in the general population. So, what does this look like in application?
As a baseline, all patients undergoing Ureteroscopy will be connected to standard monitoring, including non-invasive blood pressure, electrocardiography, oxygen saturation, and body temperature.
GENERAL ANESTHESIA
Once on the operating table in a supine position (face up), a cocktail of various drugs will be administered to induce anesthesia. The cocktail will typically consist of lidocaine, propofol, and fentanyl. Following the loss of consciousness, a muscle relaxant such as rocuronium is administered to help with intubation, which is next.
SPINAL ANESTHESIA
Once on the operating table, you will be placed into a lateral decubitus position. This position provides surgical exposure to the chest, retroperitoneum (anatomical space behind the abdominal or peritoneal cavity), hip, and lateral leg. The Anesthesiologist will then clean the skin on your back with 0.5% chlorhexidine (an antiseptic- antibacterial agent). After the skin is cleaned and dried, the Anesthesiologist will insert a 25 gauge (0.515mm) spinal needle into the space between the 4th-5th spinous process or between the 3rd-4th sinus process.
Spinous Process: a bony projection off each vertebra’s posterior (back).
Successful insertion is confirmed by aspiration of clean cerebrospinal fluid. Next, you will be administered a local anesthetic such as bupivacaine and a narcotic analgesic such as fentanyl from this spinal needle. After the injections are complete, you will be moved to a supine position (face up).
URETEROSCOPY TECHNIQUE OPTIONS
RIGID VS. FLEXIBLE
Most of the recent development in ureteroscopy has been focused on the flexible side of the business. Flexible ureteroscopes offer surgeons more flexibility and fewer complications during and after the procedure. And this makes sense based on the design of the instruments.
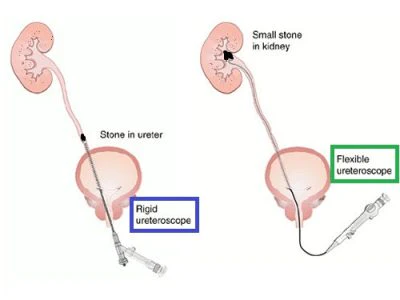
As you can see in the image above, the scope of work can be severely hindered by the rigid ureteroscope. This limitation eventually led to the development of semi-rigid ureteroscopes of various designs. These semi-rigid devices allow for the rigid application of the ureteroscope until a certain point with the addition of a flexible telescoping arm extending from the ureteroscope. Ultimately, these innovations led to the design of the flexible ureteroscope that is used in almost all ureteroscopic procedures for kidney stones today.
Studies have shown that stone-free rates after the procedure are higher with flexible ureteroscopy (SRF= 91%) than rigid ureteroscopy (SRF= 68%). Complications during the procedure were also much lower with flexible URS (9.5% of patients) versus rigid URS (25% of patients). Complications following the procedure were about the same for both flexible and rigid.
ANTEGRADE VS. RETROGRADE
Kidney stone location will play a significant role in your Surgeon’s decision to use either the Integrate or Retrograde approach. Antegrade Ureteroscopy involves the insertion of the ureteroscope following your urine flow. Retrograde Ureteroscopy inserts the ureteroscope against the flow of your urine. See below for a visual representation:
- Antegrade: Ureteroscope inserted through Kidney ➡️ Ureter ➡️ Bladder ➡️ Urethra
- Retrograde: Ureteroscope inserted through Urethra ➡️ Bladder ➡️ Ureter ➡️ Kidney
The Antregrade approach (using a flexible ureteroscope) could be possible for distal (lower) and middle ureteral stones. However, the Antegrade method has been more suitable for proximal (upper) ureteral stones and stones still in the kidney. This is due to the ability to insert the ureteroscope closer to where the stone is located (i.e., the Urologist can insert a ureteroscope into the kidney to treat a stone situated in that kidney compared to trying to reach the stone by entering the body through the urethra). However, your Urologist will make the final determination based on several factors beyond stone location.
It is important to note that the Antegrade approach requires making a puncture into your side and your kidney (much like with Percutaneous Nephrolithotomy- PCNL) to provide access for the ureteroscope and accompanying tools (lithotripter or baskets). Fortunately, there have been no significant differences in the overall complication rate between the two approaches.
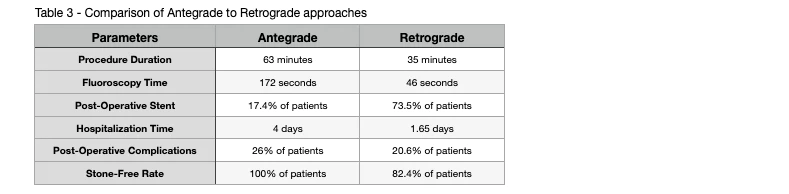
Clinical studies have revealed that the stone-free rate (SFR) was more favorable in Antegrade Ureteroscopy. However, hospital stay length was much shorter with Retrograde Ureteroscopy.
DISPOSABLE VS. RE-USEABLE URETEROSCOPES
As the use of Ureteroscopy has risen over the past few decades, Urologists and Manufacturers of these devices have expressed increasing concern relating to the cost of service. Re-usable flexible ureteroscopes are expensive instruments and have many costs associated with ongoing maintenance. To address these concerns about re-usable ureteroscopes, many types of disposable or “single-use” ureteroscopes have been introduced.
After analyzing 887 patients, no significant difference was found between the stone removal efficacy between disposable and re-usable ureteroscopes. The same can be said with regards to safety for the patient.
Many factors can influence the occurrence of post-operative infections. However, the use of disposable ureteroscopes can significantly decrease the risk of infection due to the single-use nature of the device. Unfortunately, even while proper disinfection and sterilization processes have been developed for the re-usable ureteroscopes, the re-use of medical equipment can still lead to cross-contamination.
HOLIUM VS. THULIUM LASER LITHOTRIPTER
Background
Lasers have become a fundamental aspect of the surgical management of kidney stones. The current gold standard is the Holium: Yttrium-Aluminum-Garnet (Ho: YAG) laser. However, there is much buzz around the new Thulium fiber laser (TFL). Let’s compare the two:
The Holium laser has a long history since its introduction in the 1980s (see video below). However, with recent FDA approval in 2019, the Thulium laser technology is becoming more widely available. Unfortunately, even though Thulium lasers are growing, it is still rare in most urological departments in the US.
The Thulium fiber laser (TFL) is called a “fiber laser” because its laser beam is generated inside a tiny core laser fiber (the gain medium) within the laser generator. The Holium: Yttrium-Aluminum-Garnet (Ho: YAG) uses laser rods inside resonance chambers with complex optical systems and precision alignment.
While the Holium: Yttrium-Aluminum-Garnet (Ho: YAG) lasers use laser radiation at 2100nm wavelengths, the Thulium fiber laser (TFL) uses a 1940nm wavelength, its radiation absorption is 4x higher in water. This explains its higher ablation efficiency for any kidney stone.
Ablation: removal or destruction of something from an object by vaporization, chipping, erosive processes, or by other means
Holium: Yttrium-Aluminum-Garnet (Ho: YAG) lasers are big, heavy, power-hungry machines that need dedicated high-power outlets and use noisy water cooling. Thulium fiber laser (TFL) machines are several times lighter, smaller, use quiet air-cooling mechanisms that consume less energy, and can be plugged into standard outlets.
Current super pulsed Thulium fiber laser (TFL) machines can achieve peak overs of 500W and emit very small pulse energies of 0.025 Joules and go up to 6 Joules. However, its frequency capabilities make the TFL stand out compared to the Ho: YAG laser. The current top-of-the-line Ho: YAG machines can achieve 120 Hz pulse frequency. Thulium machines can reach over 2000 Hz, and the latest commercially available can reach 2400 Hz.
Another innovation concerns pulse duration. Thulium fiber laser (TFL) machines (see video above) can be operated using very low pulse energies and very long pulse durations (up to 50 milliseconds). The very low pulse energies, higher frequencies, and longer pulse durations are features that the Ho: YAG lasers do not have. Thus, giving the performance advantage to Thulium fiber laser (TFL) machines.
Ablation Efficiency
Several studies have concluded that the Thulium fiber laser (TFL) is more efficient than the Holium: Yttrium-Aluminum-Garnet (Ho: YAG) laser. This is true even at equivalent lithotripsy settings using the same pulse energy and pulse frequency. On the “fragmentation” setting, the TFL destroys kidney stones twice as fast. On the “dusting” setting, stones are destroyed 4-5x faster than the best Ho: YAG lasers. Even comparisons between high-power Ho: YAG lasers equipped with Moses technology showed the superior performance of the TFL technology. Sometimes by a factor of three!
Moses Technology: a pulse-shape modulation that optimizes energy delivery through the water to the kidney stones compared to the application of the laser to the stone itself. It has been shown to shorten procedure time by up to 20%.
Dust Issues
The resulting kidney stone particles and fragments significantly differ between the Ho: YAG and TFL lasers. The Thulium fiber laser (TFL) is not only able to produce stone dust from all stone types, but it also produces at least twice as much dust when compared to the previously mentioned Moses Technology. The resulting average particle size is also significantly smaller with the TFL. Smaller particles require fewer basket cases to remove fragments and less risk of complication due to extended operating times.
Retropulsion
Retropulsion is the propensity of kidney stones to migrate back into the kidney while being treated. As the stone gets broken apart, the Surgeon must contend with these fragments. In addition, fragments that retreat into the kidney can become problematic if the ureteroscope can no longer reach them.
Another issue that many studies refer to is the reduced or even absent retropulsion when using the Thulium fiber laser (TFL). At equal pulse energies, the stone retropulsion threshold for TFL is four times higher than that of Ho: YAG. Retropulsion is evident with Ho: YAG laser at 0.2 Joules pulse energies, while retropulsion begins with TFL at around 1 Joules pulse energy.
This reduced retropulsion in the Thulium fiber laser (TFL) compared to the Holium: Yttrium-Aluminum-Garnet (Ho: YAG) laser is due to the lower peak power of TFL and its constant and prolonged peak power with a longer pulse duration. Thus, delivering more energy to the kidney stone being treated without sacrificing ablation efficiency.
Laser Fibers
Thulium laser fibers are smaller (150um vs. 200um for Ho: YAG), more flexible, and resistant to bending when compared to Holium: Yttrium-Aluminum-Garnet (Ho: YAG) laser fibers. One study that used exclusively Ho:YAG laser fibers with a Ho: YAG laser compared to a TFL machine using the same fragmentation and dusting parameters showed up to 90% fiber breakage with the Ho: YAG laser and no breakage with the TFL.
The smaller diameter of the TFL laser fibers has also been shown to produce smaller stone fragments. In addition, the energy density delivered is significantly higher by using smaller core diameters. This better and speedier performance by the TFL has opened the door to tackling even larger kidney stones with shorter operating times.
Safety
One of the safety features of the Thulium fiber laser (TFL) is that its laser fibers have a higher resistance to extreme bending, even when using high power. In addition, the ability of TFL to ablate kidney stones into finer particles and smaller residual fragments means fewer basket passes and complicated endoscope maneuvers that can cause additional stress during the procedure. Moreover, visibility with Thulium fiber laser (TFL) represents an extra safety feature allowing the Surgeon to judge better the position of the laser fiber tip in relation to other body parts. Better visibility also means less unintentional firing of the laser against soft tissues.
PNEUMATIC VS LASER LITHOTRIPTER
Several different energy sources are typically used during lithotripsy. And depending on where you are located around the world, the prevailing or preferred lithotripter (the device that performs stone destruction) will vary. While pneumatic lithotripsy provides high stone-free rates, there has been considerable incidence of stone migration (movement of kidney stone while work is being performed – like trying to put clothes on a child running around) has been reported.
Since the introduction of the laser lithotripter, a shift towards this energy source has been observed, especially when combined with a flexible ureteroscope. And this makes sense, as lasers provide high stone-free rates and a lower incidence of stone migration. However, this comes with an increase in procedure costs.
Operative time was significantly longer with pneumatic lithotripsy. This difference in operation time is related to the combined fragmentation and dusting technique used with laser lithotripsy. The combination of fragmentation and dusting produces smaller fragments and reduces the need to fragment retrieval with a basket or stone cone. Traditionally, fragments created due to lithotripsy needed to be removed manually using a basket instrument adding time and opportunity for complications.
Modern laser lithotripters are also smaller than their pneumatic brothers. This allows for better irrigation and vision for the Surgeon.
Upward migration of stones is a common complication when using pneumatic lithotripsy. The assault on the stone from the lithotripter can push the stone backward (see video below). There are times when a stone can even become lost in the kidney if pushed too far back. Laser lithotripsy is much more efficient in delivering power when compared to pneumatic energy sources and thus does not experience the same degree of stone migration, making it the more favored energy source in modern lithotripsy.
METHODS OF INTRODUCING FLEXIBLE URETEROSCOPE
TRADITIONAL “RAILROADING” METHOD
A double lumen ureteral catheter introduces two guide wires into the kidney. The ureteroscope is then backloaded over a second guidewire and advanced up the ureter under fluoroscopic guidance.
CYSTOSCOPE SHEATH
This is a modification of the railroading technique. A flexible Ureteroscope is introduced over a working guidewire in railroad fashion through the lumen (opening) of the cystoscope sheath.
URETERAL ACCESS SHEATH
Ureteral access sheaths provide effective and reliable access for flexible ureteroscopy. It is ideal for situations where multiple passages of the ureteroscope are anticipated since it allows for rapid entry and re-entry into the kidney’s collecting system. Access sheaths are associated with enhanced visibility for the operator due to the ability to route the irrigation fluid through the access sheath and around the ureteroscope. The rapid flow of irrigation fluid helps flush smaller stone particles out of the collecting system, allowing them to exit the sheath.
WIRELESS URETEROSCOPY
Involves the passage of a flexible ureteroscope into the ureter like a ureteric catheter without using a guidewire.
PASS URETERAL DILATION
This method utilizes the insertion of a pre-operative Double J (JJ) stent. It is beneficial in patients with abnormally narrow ureters.
MAPPING OF THE COLLECTING SYSTEM
In procedures involving stones located in the kidney (versus the ureter), understanding the anatomy of the patient’s kidney is next on the list after ureteroscope insertion. Once the ureteroscope is advanced through the Ureteropelvic Junction (UPJ- where the ureter meets the renal pelvis/kidney), the renal pelvis is inspected. The visual image from the ureteroscope is then coordinated with the images from Fluoroscopy to ensure the correct calyx is entered. Manipulations of the ureteroscope within the collecting system consist of six movements:
- Advancement
- Withdrawal
- Rotation (in either direction)
- Indeflection (increase angle)
- Undeflection (decrease angle)
PROCEDURE VARIABLES
IRRIGATION
Irrigation provides a clear view of the working area for the Surgeon by carrying away stone particles and fragments in a fluid solution. Irrigation devices are passive (gravity or pressure bag) or active (using a pump). Ideal irrigation should provide the Surgeon with a clear vision while not causing backward migration of the stone fragments (stone fragments should be propelled towards the urethra in retrograde applications).
STONE RETRIEVAL BASKETS
Retrieval baskets can be used for several different reasons. Typically they are used with a type of intrarenal lithotripsy (laser, pneumatic, etc.) when it comes time to retrieve fragments from a stone that is being destroyed. Additionally, they can be used to reposition stones to a better working location or without an intrarenal lithotripter (see video below):
In the case of stones in the ureter that are less than 10mm in size, a basket can be inserted through the urethra to grab the stone whole and remove it. However, this is a lesser-used technique as most stones less than 10mm will either pass on their own spontaneously or with the help of Expulsive Therapy (ET).
URETERAL ACCESS SHEATHS (UAS)
With the rapid technological development in flexible ureteroscopy, supporting instruments were created to increase the ease at which this treatment modality is applied. Ureteral Access Sheaths (UAS) were a product of this flurry of innovation in 1974. The primary purpose of using a Ureteral Access Sheath is to provide a method of passing the flexible ureteroscope into the ureter with greater ease.
While the performance of this instrument was poor in its early years (~20% of cases resulting in ureteral perforation), it has become an often-standard practice since the introduction of its modern form. The contemporary version features hydrophobic coating for ease of entry and hub-locking mechanisms to prevent unintended movement. With these modifications, the safety and wide use of UAS have been well-established. As a result, they have become part of the standard protocol in flexible ureteroscopy.
Let’s take a look at the impact that Ureteral Access Sheaths have on flexible ureteroscopy:
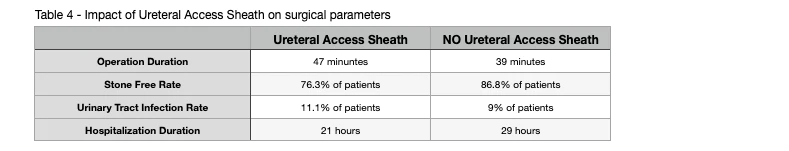
As mentioned previously, Ureteral Access Sheaths during flexible ureteroscopy allow access and evaluation of the urinary collecting system in the kidney in repeated succession. Another benefit of UAS is low intrarenal pressure (pressure inside of kidneys), superior visibility for the Surgeon, and improved drainage around the ureteroscope. The American Urological Association recommends using Ureteral Access Sheaths when performing retrograde infrarenal surgery for complex cases or those with a high volume of kidney stones.
Continued advancements in the field provided thinner and more maneuverable ureteroscopes. As a result, flexible ureteroscopy without Ureteral Access Sheaths has been developed in recent years. This development was partly due to the rapidly expanding use of flexible ureteroscopy with UAS. However, due to more frequent use, reports of adverse events began to surface. The most commonly reported issues with the use of UAS are bleeding, perforation, avulsion, and superficial ureteral mucosal wall lesions. Additionally, the use of UAS may lead to the formation of ureteral strictures and edema (swelling) of the ureteral smooth muscle, eventually leading to ureteral obstructions.
Clinical analysis has observed superficial ureteral mucosa lesions in roughly 38.8% of patients with a Ureteral Access Sheath used during their procedure. This is compared to only 4.1% of patients with superficial ureteral mucosa lesions in the procedures that did not use UAS. These findings demonstrate that Ureteral Access Sheaths can be traumatic to the ureteral wall.
NOTE: The use of disposable Ureteroscopes eliminates the risk of mucosal lesions.
When it comes to infrarenal pressure, Ureteral Access Sheaths have been shown to reduce infrarenal pressure by facilitating flow and irrigation of the kidney collecting system. However, the degree of pressure reduction may not reach sufficient levels to prevent complications associated with high intrarenal pressures during surgery, especially those procedures using pressure irrigation.
The newest ureteroscopes are thinner and allow reduced intrarenal pressure to be maintained by draining around the ureteroscopy. Older ureteroscopes were larger in diameter and limited flow and drainage. Thus, the creation of the UAS to aid these larger diameter ureteroscopes.
FLUOROSCOPY
Fluoroscopic imaging is required in conventional Ureteroscopy for stone imagine, determination of the renal anatomy, and patient safety. However, Fluoroscopy in urological procedures carries risks such as malignancy from radiation exposure to the patient, Surgeon, and operating room staff.
The main gauge of radiation exposure is Fluoroscopy time (FT) in seconds. In standard Ureteroscopy, Fluoroscopy time is variable. However, according to available data sets, 1 pulse per second Fluoroscopy time is approximately equal to a 0.01-0.02 mSv radiation dose. For comparison, a standard x-ray’s radiation dose is about 0.02 mSv. This means that one pulse in FT is the same as one x-ray image.
The National Council on Radiation Protection sets the annual maximum exposed radiation dose at 50 mSv, which means that Urologists can safely perform roughly 2500-5000 seconds of Fluoroscopy Time during a given year.
Recently urologists have investigated new methods that reduce Fluoroscopy times or have a zero-dose model in the technique. For example, in a retrospective study that included 100 patients with stones located in the kidney and ureter, a Fluoroless Urteroscopic technique was used in 50 patients. In this study, Ureteroscopy was performed using a step-by-step method. It was found that the outcomes were similar in the two groups (conventional Fluoroscopy and Flouroless). The study’s authors also reported that the Fluoroless technique was feasible and efficient for kidney and ureter stones.
In another study that evaluated a total of 350 patients, researchers concluded no difference between the two groups (Traditional Fluoroscopy & Flouroless) in terms of stone-free rate or complications. Therefore, the authors concluded that the Flouroless technique was safe and feasible.
In conclusion, the experience of your Surgeon will be the ultimate determinant of whether Fluoroscopy is used or not. For most Hospitals, Fluoroscopy is an essential part of the Ureteroscopic procedure. However, it is not mandatory for experienced surgeons.
STONE DISPLACEMENT
Modern flexible ureteroscopes have facilitated the treatment of lower pole kidney stones because of their increased deflection capability and improved visualization. However, the treatment of lower pole stones can be hampered by the decreased flexion of ureteroscopes that occurs when a laser fiber, stone basket, or grading device is in place. This may result in reduced clearance of stones and damage to the ureteroscope.
Displacement of lower pole kidney stones to more manageable locations in the kidney or ureter was first described in 2000. In a high-risk population with lower pole stones less than 20mm, it was demonstrated that the displacement of lower pole stones into a more favorable position resulted in ~7% higher stone-free rates (90% vs. 83%). The differential was even more significant for stones larger than 20mm (100% vs. 29%). These findings support the displacement method for lower pole stones before lithotripsy.
PATIENT POSITIONING
Patient position may be changed to facilitate fragment passage during ureteroscopy. For example, placing the patient in the flank position with the targeted stone side up may augment migration of stones into the renal pelvis and facilitate passage through an access sheet or into a more favorable position for extraction with a basket or another instrument.
FRAGMENTATION VS. DUSTING
Treatment goals for kidney stones are simple. First, we want the highest stone-free status after the procedure using the most minimally invasive procedure with the lowest rate of complications. The use of laser lithotripsy, when combined with flexible ureteroscopy, allows Urologists to achieve most of these goals due to the effectiveness of laser lithotripsy against all stone types.
Modern laser lithotripsy machines allow the Urologist to control laser settings (energy and frequency) and adjust the power delivered at the tip of the laser fiber. A summary of the two techniques is as follows:
- Dusting: low energy (0.2-0.5 J) and high-frequency (15-40 Hz) result in tiny fragment sizes that can pass spontaneously.
- Fragmentation: high energy (1-1.2 J) with lower frequencies (6-10 Hz) results in larger fragments that require active retrieval with baskets.
Stone fragmentation with basket extraction has been shown to have a higher stone-free rate (see video example below). And, this makes sense. When working with larger pieces of material, it is easier to identify them and remove them. However, tiny fragments or “dust” can migrate back into the kidney forcing longer operative times and increased potential for residual fragments after the procedure. In a 2019 study conducted in Egypt, researchers found the stone-free rate for fragmentation to be 78.6%, while dusting was 58.6%.
From the patient’s perspective, being free from any residual particles after a single session is much more attractive than dealing with the anxiety of waiting weeks to pass residual stone fragments. Additionally, the passage of residual stone fragments is associated with more emergency department visits for renal colic… just like passing a smaller stone normally.
However, the superior stone-free rate of the fragmentation technique is associated with longer operative times. As we’ve discussed elsewhere in this blog, longer operation durations are associated with higher complication rates. Additionally, longer operative times also come with a cost of $29-$80 per minute of the procedure.
This can add up! In the Egyptian study mentioned above, the operative time in the dusting group was 75.8 minutes and 91.2 minutes in the fragmentation group. That’s a difference of 15.4 minutes or $446.60-$1,232.
On top of this, the fragmentation technique also required Ureteral Access Sheaths (UAS) and extraction baskets to remove the fragments. The cost of these instruments can add to the already higher price of this technique.
The main advantage of the dusting technique (see video below) is the ability to complete the procedure during a single pass of the flexible ureteroscope that can be done over a guidewire. Therefore, using a Ureteral Access Sheath (UAS) is significantly lower with this technique. This translates into the avoidance of intra-operative complications and substantially shorter operative times.
On the other hand, working without a UAS can lead to an increase in intra-pelvic pressure. This is the most probable cause for the development of septic shock requiring ICU admission in some surgeries.
Finally, the stone-free rate of the dusting technique was significantly lower than that of the fragmentation method due to the inability to be sure that a stone is completely dusted due to the numerous tiny fragments. Ultimately, your Surgeon’s preference will determine the type of stone destruction technique used.
TWO SHIFT VS SINGLE PLAYER MODE
Laser lithotripsy is a time-consuming process. And, with the rise of kidney stones worldwide, the volume of these procedures is also rising. During a ureteroscopic procedure, the Surgeon has to hold the Ureteroscopy and focus on the target (kidney stone), all while standing in the same position. Ureteroscopy procedures can last upwards of an hour. Standing in the same position can ultimately lead to the Surgeon’s discomfort. They may also negatively impact the performance of the procedure.
Fortunately, teamwork can overcome this fatigue, where two surgeons split the workload to provide better ergonomics and performance for the patient.
POST-OPERATIVE STENTING
Stent insertion affects Ureteroscopy is a common and widely accepted best practice for pregnant patients who have a solitary kidney, transplanted kidney, or renal impairment. The use of a stent is also necessary for complicated ureteroscopic procedures involving bleeding, ureteric trauma, or sizeable residual stone burdens. However, there is no consensus on whether or not a stent should be used after an uncomplicated procedure.
Despite the controversy, most urologists today routinely use stents. The hypothetical notion justifies that stent placement promotes the passage of residual stone fragments and clots, lowers the risk of ureteral stricture formation, prevents obstructions, and prevents renal colic resulting from ureteric edema following stone retrieval.
However, stent insertion after Ureteroscopy may potentially be associated with specific morbidities such as:
- Pain
- Infection
- Irritative voiding symptoms
- Upward stent migration
- Sepsis
- Forgotten or encrusted stents
The frequency and severity of these complications may be reduced by using a double pigtail stent with an extraction string. The extraction string allows for fast, non-invasive stent removal. Randomized prospective trials have found that routine stunting after an uncomplicated procedure is unnecessary and that stenting may be associated with higher morbidity. Uncomplicated is defined as having the stone fragmented and extracted without ureteric injury.
FACTORS INFLUENCING OPERATION DURATION
To help better understand the different factors that influence operation durations, we will look to a research study from the United Kingdom from 2020. This study evaluated 736 patients over 6.5 years.
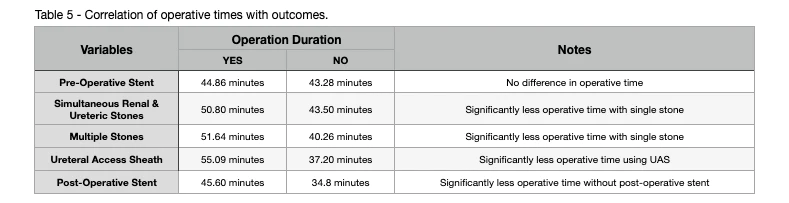
As you can see by the data in Table 5 above, treatment of multiple renal stones, ureteric and renal stones (i.e., stones in both the ureter and kidneys), large stones, and the use of access sheath were all associated with longer operation times. In addition, while there was no difference in the operative time with pre-operative stents, patients without post-operative stents enjoyed significantly lower operation durations. This is important because as operative time increases, the risk of higher grade Clavien-grade complications (see next section) increases.
When it comes to larger stones (15mm+), it is well known that these stones need longer procedural times. However, it is difficult to determine a point at which the procedure time becomes too long, and the risks become unmanageable. To help us better understand this, we will look to a retrospective study performed in Japan of over 12,000 Ureteroscopy patients. In this study, the researchers determined that a cut-off time over 90 minutes significantly increased injuries and mortality rates.
COMPLICATIONS
Various complications may be encountered during and after a ureteroscopy procedure. Unfortunately, Ureteroscopy is not as innocent as expected. Two of the most frequently reported complications are infectious processes and ureteral damage. As with other dendrological procedures, operations should not be performed until infections are treated with the appropriate antibiotics, and the urine has returned to sterile.
While no definitive safe operating time has been established, as the operative time increases, so does the risk of post-operative infections. A study performed by Deemir et al. reported that prolonged operation time was an independent risk factor for post-operative fever and/or infection. The study also concluded that infectious complications increased 11x if procedures exceeded 61 minutes.
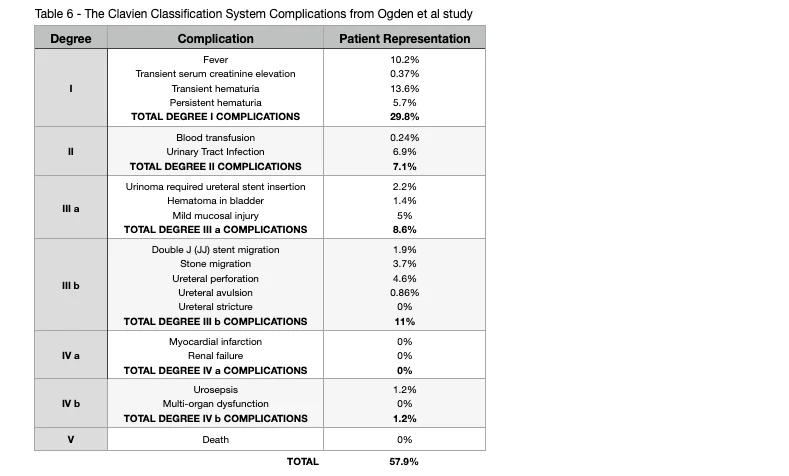
CLAVIEN SCORING SYSTEM
Ureteroscopy is considered a safe procedure. However, as with any surgical procedure, it may result in certain complications both during and after. The Clavien classification system was developed to help better assign complications to a structured system that would allow practitioners worldwide to speak the same language in terms of surgical complications. The classification system is outlined below:
LOWER POLE KIDNEY STONES
Treatment of lower pole kidney stones presents a challenge for Urologists. Limitations of the deflection capabilities (angles at which the device can be contorted to navigate the urinary tract or kidney) of the single deflection ureteroscope make it difficult for surgeons to navigate the problematic angles required to gain access to stones in the lower pole of the kidney. In addition, even when the ureteroscope can be positioned to access the lower pole, the placement of instruments (such as laser fibers) in the working channel can decrease the maximum angle of deflection and prevent access or examination of the stone burden. This limitation of ureteroscopy has led to the development of a dual deflection Ureteroscopy.
Dual deflection ureteroscopes have a sound, more proximal, unidirectional deflection point controlled with a separate lever. This Ureteroscopy can achieve greater overall deflection and thus may be of significant benefit in managing lower pole kidney stones. These new flexible ureteroscopes can now access the lower pole of the kidney in 93% of cases.
Selection of treatment modality for a lower pole kidney stone requires an informed conversation with the patient about the risks, benefits, and stone-free rates of the various available procedures. The treatment choice will also depend on the surgeon’s preferences and level of expertise.
STAGHORN KIDNEY STONES
Staghorn kidney stones are large-branched stones that occupy a majority of the kidney collecting system. Staghorn stones can either be classified as complete or partial based on the extent of the occupied collecting system (see photo below). Most staghorn stones are of mixed stone composition and are related to infection or other metabolic conditions.
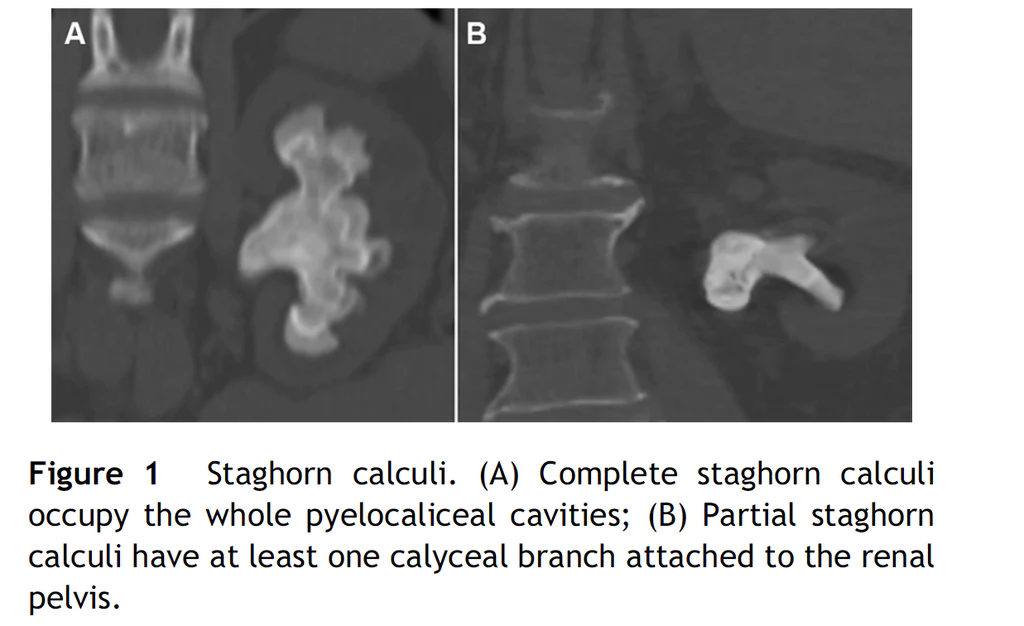
Over the past decades, Percutaneous nephrolithotomy (PCNL) has been the mainstay treatment for staghorn kidney stones. However, Ureteroscopy has been on the rise due to the advancements in this field.
In a review of five studies conducted by the Urology Department of the University Hospital of Zurich (Switzerland), researchers found that up to four ureteroscopy sessions with an average operative time of 99 minutes per session resulted in a stone-free rate of 53% for complete staghorn kidney stones. In a group of patients with partial staghorn stones, up to three sessions with an average operative time of 90 minutes per session yielded a stone-free rate of 47%. Additionally, complications such as fever, sepsis, extravasation, and subcapsular hematoma occurred in 59% of complete staghorn patients and 26% of partial staghorn patients.
The American Urological Association (AUA) currently recommends Ureteroscopy only as a second choice for stones larger than 20mm (2cm). Percutaneous Nephrolithotomy is the first-line recommendation.
KIDNEY STONES LARGER THAN 20MM
Despite the successful and safe outcomes enjoyed in the Ureteroscopic management of kidney stones between 1-2cm, the treatment for larger stones (> 2cm) continues to be challenging. As such, Percutaneous Nephrolithotomy (PCNL) is the preferred treatment method with highly successful outcomes in a single session. However, given the invasive nature of this procedure, complications such as bleeding and infection have left urologists to seek less invasive alternatives.
Technological innovations coupled with experience gained in semi-rigid ureteroscopic stone management have made it possible to perform flexible Ureteroscopy safely and efficiently on a majority of kidney stones. However, despite comparable stone-free rates observed with stones less than 20mm, reported data demonstrates that as stones get larger, stone-free rates drop along with an increased need for additional sessions. Therefore, the overall success of this procedure for stones larger than 20mm depends mainly on the operator’s experience.
As a result, the American Urological Association recommends Percutaneous Nephrolithotomy (PCNL) as the preferred treatment modality for stones that are larger than 20mm and complex stones. However, despite higher stone-free rates obtained in a single session, the risk of severe complications during and after the procedure points to the more invasive nature of PCNL. Additionally, PCNL may not prove to be the technique of choice for morbidly obese individuals or those with bleeding disorders.
In light of the invasive nature of Percutaneous Nephrolithotomy and the host of potentially serious complications associated with the procedure, Urologists have begun to seek less invasive alternatives such as flexible Ureteroscopy. Particularly in the less invasive treatment of larger kidney stones.
The success rate obtained with flexible ureteroscopy for kidney stones larger than 20mm has been reported as 77% after a single session and 93% with additional sessions as needed. These results are comparable to those achieved with Percutaneous Nephrolithotomy. However, stone-free rates for lower pole stones after flexible Ureteroscopy are still lower in the range of 62-85%. For stones larger than 40mm, the success rate dropped to 50%, with an average of two sessions required.
In light of the currently available data, it is clear that flexible Ureteroscopy can be performed successfully with acceptable complication rates for stones larger than 20mm. However, to obtain the desired stone-free rate, patients need to be well informed about the need for multiple staged procedures and thoroughly evaluate their stone size and location in their kidneys.
PROCEDURE PERFORMANCE
As mentioned in the patient selection section, the overall success of Ureteroscopy will primarily be affected by both stone size and location. As such, please see Table 6 for a pooled analysis of multiple studies to provide an average stone-free rate based on stone location and size:

CONCLUSION
As you can see by the data, Ureteroscopy is a safe and effective minimally invasive procedure (retrograde approach only) for the treatment of:
- Complicated ureteral stones (moderate to server hydronephrosis and/or uncontrolled pain)
- Kidney stones that were not destroyed with Shockwave Lithotripsy (SWL)
- Lower pole kidney stones less than 20mm
- Kidney stones where Percutaneous Nephrolithotomy (PCNL) is not an option
- Kidney stones in the ureter of pregnant patients
- Kidney stones in the setting of uncorrected bleeding or in patients who require continuous anticoagulation/anti-platelet therapy.
It is important to keep in mind that for uncomplicated stones less than 10mm located in the ureter, Expulsive Therapy (ET) is strongly recommended by the American Urological Association. There will be times that Urologists will recommend Ureteroscopy for uncomplicated stones less than 10mm in size and this should be challenged!
Thank you for reading!
Please leave any comments or questions below ????

Comments or questions?
Responses
WHAT TO READ NEXT
Publish Date: December 3, 2023
The Stent Survival Guide
Publish Date: March 28, 2022
American Urological Association (AUA) Guidelines for the Treatment of Kidney Stones
Publish Date: March 20, 2022
Percutaneous Nephrolithotomy (PCNL) for Kidney Stones